Preliminary results from a Phase 2 clinical trial of the R21/MM malaria vaccine candidate by researchers from the University of Oxford and the Clinical Research Unit of Nanoro show a 77% efficacy rate among 450 test subjects between the ages of 5-17 months in Burkina Faso. The only currently available malaria vaccine on the market, the RTS,S/AS01, which was launched by GlaxoSmithKline in 2016 and is more popularly known as Mosquirix, only has an efficacy rate of around 55%, with booster shots required on an annual basis. Given that malaria killed an estimated 409,000 people in 2019 and infected more than 229 million, this is a significant development, especially considering that children under the age of 5 accounted for 67% of malaria deaths in 2019. It is of particular significance to Africa, which alone makes up roughly 94% of malaria cases and deaths around the world.
Vaccinating against malaria has proved to be a huge challenge to overcome for researchers, given that it is caused by a parasite, not by a bacterium or a virus. Moreover, unlike other diseases, it is possible to contract malaria more than once, as catching malaria doesn’t prompt a strong enough antibody response and naturally acquired immunity diminishes after just a few years. Furthermore, “exposing the body to a dead or attenuated version of the disease agent”, which is often used as a method to develop vaccines for other diseases, is ineffective for malaria.
Given that Novavax and the Serum Institute of India (SII), both huge pharmaceutical companies who have also developed COVID-19 vaccines, have formally declared their interest in the newest vaccine candidate, there are certainly promising signs ahead. In fact, the two companies are co-developing the R21/MM. Novavax holds a proprietary license for the Matrix-M component of the vaccine candidate, which boosts the body’s immune response and is also used in its COVID-19 vaccine. The R21 component was developed by the University of Oxford, which also developed the AstraZeneca COVID-19 vaccine. Meanwhile, the license to the vaccine is held by the SII.
The results from the Burkina Faso trial have thus been warmly received by professionals from around the world. For instance, the director of the World Health Organization’s (WHO) Global Malaria Programme, Pedro Alonso, described it as “very positive news.” He did add, however, that “This is a trial with 450 children. … We are still quite far away from having the type of information that would allow us to get very excited.”
Nevertheless, given that the WHO’s minimum ‘target efficacy’ for malaria vaccines is 75%, preliminary results from Phase 2 trials of the R21/MM represent a historic achievement.
Keeping this in mind, Rwanda Biomedical Centre’s (RBC) Director-General, Dr. Sabin Nsanzimana, said, “With such developments, we get hopeful that something new is going to be added to the existing efforts for fighting against malaria. When we look at how quickly the vaccines for Covid-19 have been developed, it gives hope that even one for malaria can be found within a time that is not very far.”
To Alonso’s point of it being very early on, researchers are currently recruiting for the launch of Phase 3 trials that will prospectively involve 4,800 children in Burkina Faso, Mali, Kenya, and Tanzania. It is thought that data from that trial could be presented to regulators in 2022, who could then approve the vaccine candidate by early 2023. There is also hope that emergency use authorisations even before that.
It is estimated that billions of dollars are spent on malaria every year by actors around the world in terms of treatment, nets, insecticides, antimalarial drugs, healthcare staff and facilities, medical equipment. Furthermore, it is thought that malaria costs Africa’s GDP at least $12 billion every year. In this context, it is thought that the R21/MM could save billions and maybe even generate and inject billions into the African continent.
Malaria Vaccine Candidate Shows 77% Efficacy in Potentially Historic Outcome for Africa
Given that Africa alone accounts for 94% of malaria cases and deaths, promising results from Phase 2 clinicals trial of the R21/MM malaria vaccine candidate could foreshadow a landmark moment.
April 30, 2021
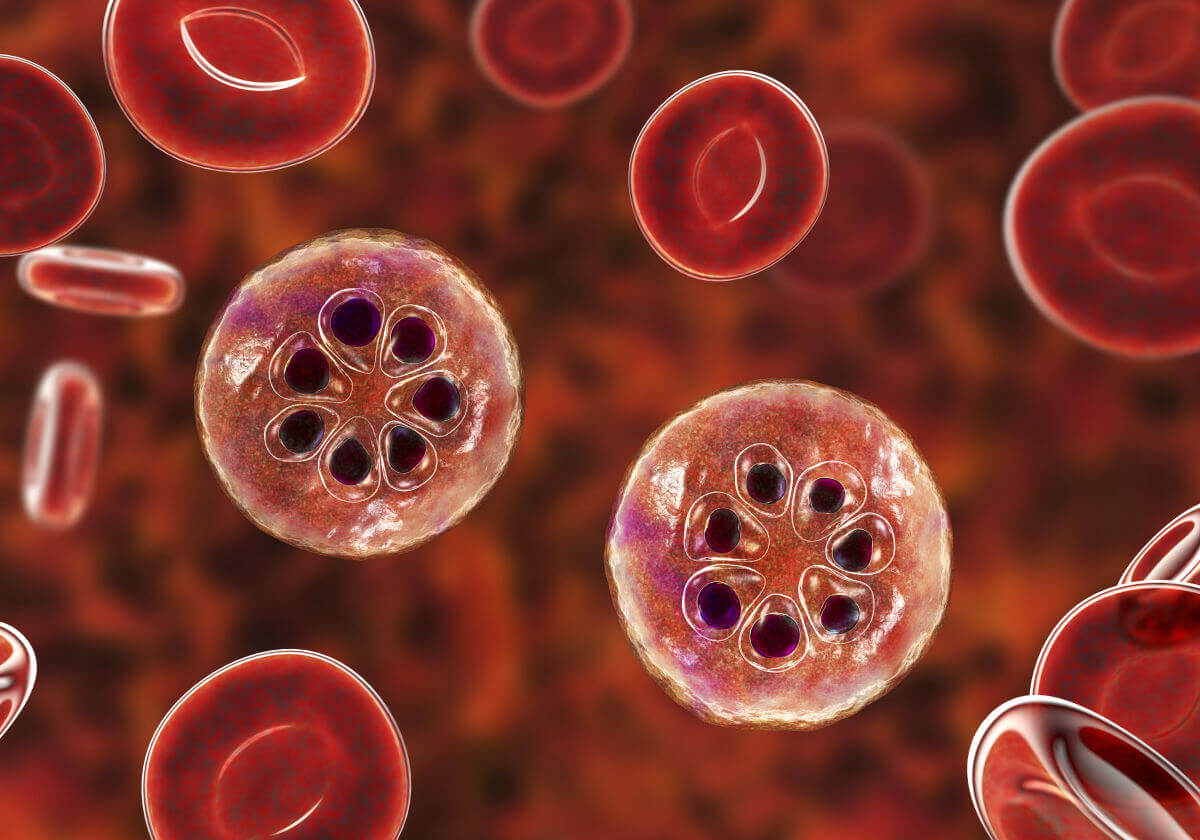
IMAGE SOURCE: DR_MICROBE VIA GETTY IMAGESIt is estimated that billions of dollars are spent on malaria every year by actors around the world in terms of treatment, nets, insecticides, antimalarial drugs, healthcare staff and facilities, medical equipment.
